Anesthetics in Ophthalmic practice

 PH dependent for Anesthetics in Ophthalmic Practice:
PH dependent for Anesthetics in Ophthalmic Practice:
(less effective at low pH like inflamed tissue)
Classes ( esters and amides)

hydrolyzed by plasma cholinesterase
metabolized in liver
Examples
cocaine
tetracaine (amethocaine)
proparacaine
procaine
benoxinate

longer duration and less systemic toxicity
metabolized in liver
Examples
lidocaine
mepivacaine
bupivacaine
Routes of administration
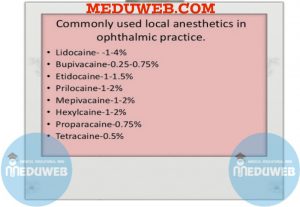
 Topical Anesthetics in Ophthalmic Practice:
Topical Anesthetics in Ophthalmic Practice:
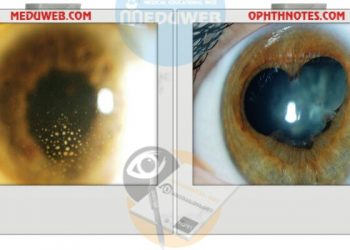
Disturb intercellular junction of corneal epithelium (increase permeability)
Examples
Proparacaine (Ophthaine)
• 10- to 30-minute duration
• cause allergic dermatitis
Tetracaine (Pontocaine)
•similar to proparacaine but longer duration
• more toxic to corneal epithelium
Benoxinate
• similar to proparacaine
• can be combined with fluorescein (Fluress) for tonometry
Cocaine
• greatest epithelial toxicity
• excellent anesthesia
• sympathomimetic effect (test for Horner’s syndrome)
 Parenteral( injectables) for Anesthetics in Ophthalmic Practice:
Parenteral( injectables) for Anesthetics in Ophthalmic Practice:
May be used with epinephrine (1:100,000) to increase duration by preventing systemic absorption and decreases bleeding
Hyaluronidase (Wydase) 150 IU increases tissue penetration, but decreases duration.
Side effect of retrobulbar anesthesia 1⁄4 respiratory depression, bradycardia
Toxicity: hypotension, convulsions, nausea, vomiting
Examples
Lidocaine (Xylocaine)
• 1 hour duration (2 hours with epinephrine)
• used for local anesthesia and akinesia
Procaine (Novocain)
• 30 to 45 minute duration
Mepivacaine (Carbocaine)
• 2 hours duration
Bupivacaine (Marcaine)
• 6 hours duration
 General Anesthetics in Ophthalmic Practice:
General Anesthetics in Ophthalmic Practice:
All agents decrease intraocular pressure (IOP)except ketamine, chloral hydrate, N2O, and ether
Malignant hyperthermia (Major complication)






Anesthetics in Ophthalmic practice power point presentations:
Ophthalmic anesthesia:
Anesthetics in ophthalmic practice videos
Ophthalmic anesthesia towards a better block video
Regional anesthesia video
Anesthetics in Ophthalmic practice












Discussion about this post